Varicose veins - Medical maneuvers and surgical skils
varicose veins - Medical maneuvers and surgical skils
Sours : Lecturio 2024
Varicose veins are a common condition where veins, particularly in the legs, become enlarged, swollen, and twisted, often appearing blue or dark purple through the skin. They can cause discomfort, aching, and a heavy feeling in the legs, especially after standing for long periods. While they are usually not dangerous, they can sometimes lead to complications like ulcers or blood clots. Treatment options range from self-care measures, such as exercise and elevation of the legs, to medical procedures like sclerotherapy, laser therapy, or surgery. It's important for individuals with varicose veins to consult healthcare professionals for proper diagnosis and treatment plans.
Definition:
Chronic venous disease encompasses a range of conditions characterized by venous dilation and/or abnormal vein function in the lower extremities, primarily resulting from venous hypertension.
Epidemiology:
More prevalent in females than males.
Lifetime incidence of chronic venous disease affects up to 50% of individuals.
Lifetime incidence of chronic venous insufficiency: Up to 40% in women
Up to 17% in men
Incidence increases with age.
Lifetime incidence of chronic venous disease affects up to 50% of individuals.
Lifetime incidence of chronic venous insufficiency: Up to 40% in women
Up to 17% in men
Incidence increases with age.
Etiology:
Chronic venous hypertension is the underlying cause. Causes of venous hypertension include:Obstruction, typically due to deep vein thrombosis (DVT).
Reflux, often resulting from valve incompetence, which may develop following obstruction. Primary disease (symptomatic presentation without a precipitating event) accounts for 70%. Secondary disease (develops after DVT obstruction) accounts for 30%. Risk factors for chronic venous insufficiency include:
Increased age
Higher BMI
Family history of venous disease
Ligament laxity (hernias, flat feet)
Prolonged standing
Smoking
Previous DVT
Klippel–Trenaunay syndrome
Elevated estrogen states, such as pregnancy.
Reflux, often resulting from valve incompetence, which may develop following obstruction. Primary disease (symptomatic presentation without a precipitating event) accounts for 70%. Secondary disease (develops after DVT obstruction) accounts for 30%. Risk factors for chronic venous insufficiency include:
Increased age
Higher BMI
Family history of venous disease
Ligament laxity (hernias, flat feet)
Prolonged standing
Smoking
Previous DVT
Klippel–Trenaunay syndrome
Elevated estrogen states, such as pregnancy.
Pathophysiology:
Venous hypertension, stemming from DVT or primary valve incompetence, leads to:Increased venous pressure in deep veins
Elevated pressure in perforating veins
Heightened pressure in superficial veins DVT causes endothelial dysfunction, initiating chronic inflammation and eventual remodeling of vein walls, characterized by:
Increased Type 1 collagen
Decreased Type 3 collagen
Reduction in smooth muscle cells
Degradation of the extracellular matrix
Elevated proteinases resulting in increased permeability. Severe wall dysfunction raises the risk of DVT due to:
Impaired blood movement (stagnation)
Chronic inflammation and endothelial damage
Elevated pressure in perforating veins
Heightened pressure in superficial veins DVT causes endothelial dysfunction, initiating chronic inflammation and eventual remodeling of vein walls, characterized by:
Increased Type 1 collagen
Decreased Type 3 collagen
Reduction in smooth muscle cells
Degradation of the extracellular matrix
Elevated proteinases resulting in increased permeability. Severe wall dysfunction raises the risk of DVT due to:
Impaired blood movement (stagnation)
Chronic inflammation and endothelial damage
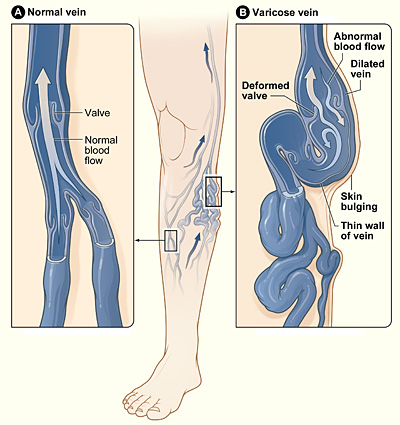
Varicose veins
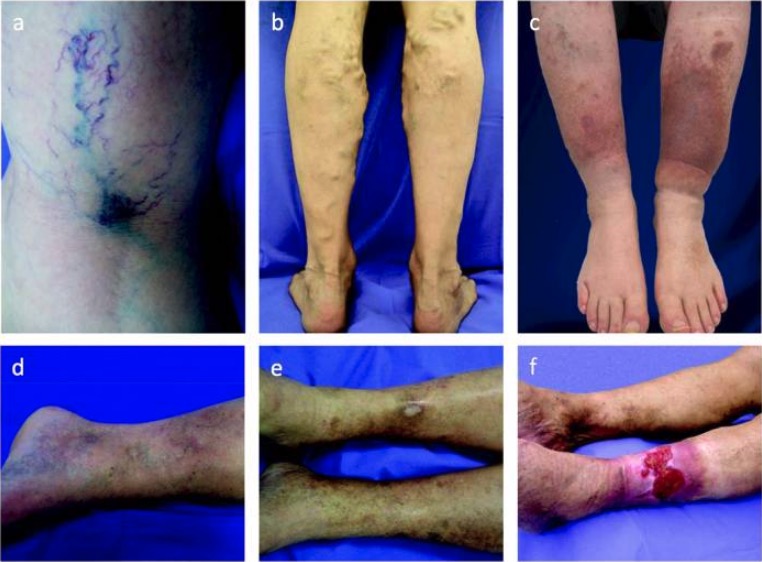
Image: “Varicose veins” by National Heart Lung and Blood Institute. License: Public DomainSkin and Soft Tissue Changes:
The escalation of venous hypertension coincides with heightened vessel permeability. This results in the outflow of blood components into the subcutaneous space, leading to a cascade of effects:- Fluid → edema → increased pressure in the extremity, potentially resulting in:
- Necrosis
- Hindered lymph drainage → further fluid buildup and compromised waste removal
- Red blood cells (which degrade) → deposition of hemosiderin → skin pigmentation
- Proteinases → formation of cutaneous ulcers
- White blood cells → release of cytokines → subcutaneous fibrosis (lipodermatosclerosis) → decreased capillary density in affected areas:
- Manifesting as white plaques (atrophie blanche)
- Reduced blood flow → impaired healing and ischemia/necrosis
Clinical Presentation:
Manifestations of chronic venous disease vary along a spectrum:- Asymptomatic venous dilation
- Mild disease:
- Telangiectasias
- Reticular veins
- Varicose veins
- Mild dependent ankle edema
- Severe disease (chronic venous insufficiency):
- Marked edema
- Skin alterations
- Ulcers
Presenting Symptoms:
- Dependent pitting edema- Lower extremity discomfort or pain:
- Often described as "heavy legs," throbbing, aching, or cramping
- Exacerbated by standing
- Unlike peripheral artery disease (PAD), pain alleviates with leg elevation or walking
- Numbness or tingling
- Pruritus
- Visible tortuous veins:
- Telangiectasias: intradermal venules < 1 mm in diameter
- Reticular veins: subdermal veins, 1–3 mm in diameter
- Varicose veins: subcutaneous veins > 3 mm in diameter
- Skin changes:
- Discoloration of skin (brown or blue-gray) due to hemosiderin deposits
- Stasis dermatitis (eczematous rash) characterized by:
- Erythema
- Scaling
- Weeping
- Erosions
- Crusting
- Lipodermatosclerosis:
- Firm, indurated areas
- Adhesion of skin to subcutaneous tissue (subcutaneous fibrosis), often prominent at the medial ankle and may form a constrictive band
- Atrophie blanche:
- Atrophic white plaques with red punctate dots or telangiectasias
- Circular or stellate shape
- Surrounded by hyperpigmentation
- Ulcers: commonly located over the medial malleolus
Diagnosis and Classification:
Physical Examination:
Lower extremity assessment may reveal:
- Edema
- Visible or palpable tortuous superficial veins
- Characteristic skin changes
- Ulcers may or may not be present
Venous Refilling Time:
- Observing the time it takes for visible veins to distend after the patient stands from a seated position.
- A refilling time of 20–40 or < 20 seconds is considered abnormal.
Ankle–Brachial Index (ABI):
- Calculated as the ratio of blood pressure at the ankle to blood pressure at the arm.
- An ABI ≤ 0.9 suggests peripheral artery disease (PAD).
- Note: Compression therapy, standard in venous insufficiency, is contraindicated in PAD.
Imaging:
Duplex Ultrasonography:
- First-line test to:
- Confirm the diagnosis if uncertain
- Determine the etiology
- Exclude deep vein thrombosis (DVT)
- Assess severity of deep vein disease
- Localize affected anatomy
- Combines B-mode imaging of deep and superficial veins with Doppler assessment of blood flow.
- Obstruction is indicated by absence of blood flow and noncompressible veins.
- Reflux is indicated by reversal of blood flow (> 0.5 seconds in superficial and perforator veins, > 1 second in deep veins).
Cross-Sectional Venography with CT or MRI:
- Utilized to assess the deep venous system, particularly in areas poorly accessible by ultrasound (e.g., infrainguinal area).
- Considered when ultrasound results are inconclusive or normal.
Catheter-Based (Invasive) Venography:
- Gold standard but rarely necessary for diagnosis.
- Typically reserved for cases requiring more invasive intervention.
Clinical, Etiologic, Anatomic, and Pathophysiologic (CEAP) Classification of Chronic Venous Disease:
Clinical Signs:
- C0: No visible or palpable disease
- C1: Telangiectasias and reticular veins
- C2: Varicose veins
- C3: Edema
- C4: Skin changes
- C4a: Pigmentation or stasis dermatitis
- C4b: Lipodermatosclerosis
- C5: Healed ulcer
- C6: Active ulcer
- C6R: Recurrent active ulcer
Etiologic Signs:
- Ep: Primary causes, typically valve degeneration leading to reflux
- Es: Secondary causes, usually DVT or trauma
- Ec: Congenital causes
Anatomic Signs:
- As: Superficial veins
- Ad: Deep veins
- Ap: Perforating veins
Pathophysiologic Signs:
- Pr: Venous reflux
- Po: Venous obstruction
- Pr,o: Both reflux and obstruction
Management:
Goals:
- Reduction of edema.
- Alleviation of discomfort.
- Prevention and treatment of skin manifestations.
- Healing of ulcers.
- Improvement of modifiable risk factors.
Conservative (Nonsurgical) Management:
- Frequent leg elevation (30 minutes, 3–4 times daily) to enhance venous drainage.
- Exercise to enhance calf muscle pump function.
- Weight loss to decrease pressure.
- Skin care:
- Cleansing.
- Emollients to maintain skin barrier, prevent dryness and fissuring, and reduce scratching (which can lead to ulcers).
- Compression therapy (hosiery):
- Primary initial management technique, but contraindicated with coexisting peripheral artery disease (PAD).
- Requires long-term adherence.
- Venoactive substances to increase venous tone:
- Used in patients with resistant edema despite compression therapy or contraindications to compression therapy.
- Options available in the United States include escin (horse chestnut seed extract) and micronized purified flavonoid fraction.
- Ulcer care:
- Debridement to remove surrounding necrotic tissue, promote healthy granulation tissue, enhance reepithelialization, and reduce infection risk.
- May be done using surgical, enzymatic, or biologic methods.
- Topical agents such as cadexomer iodine and silver sulfadiazine may be used, but most do not improve healing rates.
- Systemic antibiotics are reserved for patients with acute cellulitis or clinically infected ulcers.
- Dressings.
- Medical options for treating resistant ulcers include stanozolol (an anabolic steroid that stimulates fibrinolysis) and pentoxifylline (to increase microcirculation and tissue oxygenation).
Surgical Management:
Goals:
- Occlusion or removal of damaged vessels and restoration of proper blood flow.
- Reduction of venous hypertension to alleviate edema and skin effects.
Options include:
- Superficial venous ablation (thermal destruction).
- Sclerotherapy (injection of substances causing fibrosis and occlusion).
- Phlebectomy (vein excision).
- Angioplasty and stenting to relieve obstructions in the deep veins.
- Valve repair in deep veins.
Complications:
- Bleeding from varicose veins.
- Deep vein thrombosis (DVT).
- Superficial thrombophlebitis, treated with NSAIDs and compression therapy.
- Cellulitis or infected ulcers, requiring systemic antibiotics and debridement, which may lead to amputation.